|
"TMJ" is a popular buzzword in our society which, in reality, is an acronym for an anatomical body part, the temporomandibular joint. "TMJ" is not a syndrome, nor a disease, but is merely a designation for the human jaw joint. To say someone "has TMJ" is the same as saying someone "has knee". TMJ disorders are a major cause of facial pain and dysfunction and are an important and appropriate focus of attention by health care providers. TMJ disorders consist of a family of problems that relate to your jaw joint complex. These problems involve complicated anatomical structures such as muscles, ligaments, tendons, the mandible (lower jaw), teeth, nerves, blood vessels and other structures. When your TMJ and associated structures are in good health, the jaws open and close smoothly and comfortably in talking, chewing, and use in other functions.
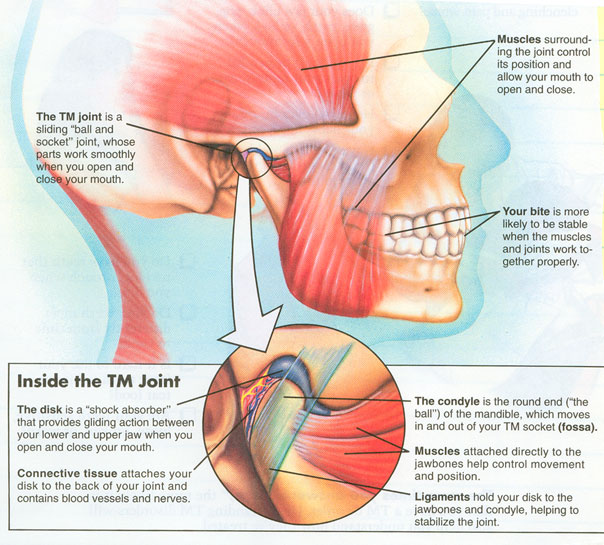
Anatomy of TMJ
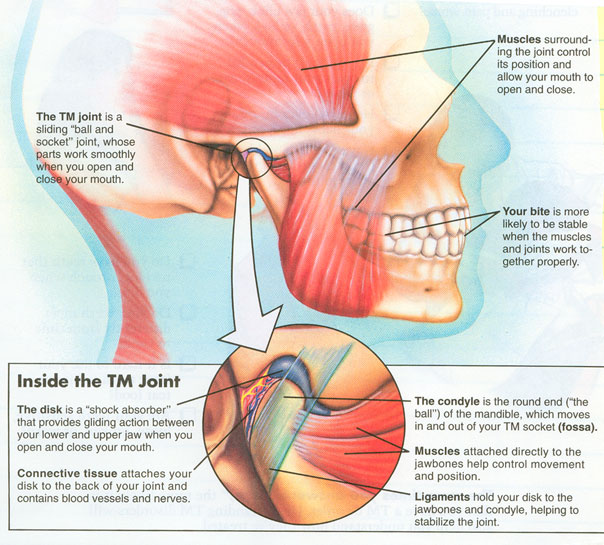 Complex Masticatory Muscles - Surrounding the joint are groups of muscles that contract and relax in harmony so the jaws function properly. When the muscles are relaxed and flexible, and not under stress, they work in harmony with the other parts of the TMJ complex. Complex Masticatory Muscles - Surrounding the joint are groups of muscles that contract and relax in harmony so the jaws function properly. When the muscles are relaxed and flexible, and not under stress, they work in harmony with the other parts of the TMJ complex.
Teeth and Occlusion - The way the teeth fit together may affect the TMJ complex. A poor occlusion (bite relationship) may cause the muscles to malfunction and ultimately cause damage to the joint itself. A stable occlusion with good tooth contact and interdigitation provides maximum support to the muscles and joint. Instability of the occlusion can increase the load or pressure on the joint causing damage and degeneration.
Temporomandibular Joint - The temporomandibular joint is the joint where the lower jaw articulates with the base of the skull and allows movement of the lower jaw. This joint is made up of the mandibular condyle which is the round end of the mandible that moves and rotates during talking, eating, etc. The temporal fossa is the socket where the condyle fits. The disc or meniscus is situated between the condyle and fossa and is made up of cartilage-like dense collagen. It provides the sliding action between the lower jaw and the fossa (or top part of the joint). Ligaments hold the disc to the condyle and help stabilize the joint. Connective tissue holds the disc to the back of the joint and contains blood vessels and nerves. Connective tissue also forms the joint capsule which surrounds the joint. The illustration above demonstrates the "normal" relationship of the disc to the surrounding joint structures. While many patients may have discs that are displaced from this position and NOT have any symptoms, it is very common that those who have TMJ pain and dysfunction also have displaced discs. It is therefore likely that this displacement plays a significant role in the development of such problems.
Causes of TMJ Disorders
Trauma or injury to the jaw - This can cause injury to the joint in the form of fracture to the condyle, torn ligaments, torn cartilage, displacement of articular discs, damage to muscles and other injuries.
Diseases - Certain diseases such as rheumatoid arthritis can effect the joint surfaces and certain muscular diseases can effect function.
Stress - This is often the cause of TMJ pain. Stress can be manifested by clenching and overstressing the muscles and jaw joints. This can be seen as pain, muscle spasm, and damage to the joints.
Habits - Bruxism (grinding the teeth, especially at night) can cause muscle and joint problems.
Bite or occlusion problems - Malaligned teeth, missing teeth, and malalignment of the jaws can create an imbalance of muscular and joint function which can lead to discomfort and joint damage.
Dental and Medical Evaluation
The first step to arriving at a treatment plan involves a fact-finding program. This collects the necessary information to arrive at a diagnosis.
Dental and Medical History - This provides information about your overall health, any history of accidental injuries, symptoms you are experiencing, treatment you have received, medication you are taking, and much more. It helps determine lifestyle, habits, stress factors, and family history. All of this information is important.
Physical Exam - This helps identify your symptoms and malfunctions. It may involve examination of your muscles and joint for tenderness. Jaw function is carefully measured. The joint can be examined for noises and sounds by various listening devices. Your teeth and occlusion may be examined to determine the stability of your bite.
Imaging Tests - A variety of tests help confirm or rule out a diagnosis of temporomandibular joint disorders. Various x-rays (tomograms, transcranials, and others) show an image of bony contours of the joint. These films may reveal fractures, tumors, or damage to the bony surfaces of the joint. A MRI (magnetic resonance imaging) produces images of both hard and soft tissues and may reveal damage or displacement of the disc or ligaments.
Dental Casts - These are models of your teeth that may help determine if there is instability of your bite in relation to your disorder. It may also reveal a joint disorder that has effected the way your teeth fit and line up.
Diagnosis
A good diagnosis is of primary importance so that the proper treatment may be precisely directed to the correct TMJ dysfunction.
Extracapsular disorders - These are disorders that exist outside the joint itself. These patients often have little or no mechanical problems within the TMJ but suffer the effects of the structures outside of the joint.
Myofascial pain dysfunction - This is the most common TMJ dysfunction and usually involves muscle imbalance with muscle spasm and pain. This has a multitude of causes such as stress, grinding of teeth, instability of the bite and others.
Diseases and pathology of the surrounding area - This can include tumors of the jaw, salivary glands, and associated structures, neurological disorders, systemic disorders effecting the head and neck, and referred pain from the neck, back, and associated structures.
Internal joint disorders - Damage or disease to the joint itself such as the disc, condyle, ligaments, or synovium (lining of the joint).
Disc displacement - A displaced disc may cause popping and clicking due to the disc being displaced forward so that the condyle clicks or pops in its translation during opening. A displaced disc may block the condyle from translating forward during opening and restrict the opening. This is sometimes called a "closed lock".
Adhesions - Scar tissue may have developed between the condyle and disc or the disc and the fossa that restricts jaw movements.
Disc perforations (holes or tears in the disc) - This occurs when the disc is torn or worn through by continual overloading of the joint. This often causes a grinding sensation or gravel-like sound.
Arthritic conditions - Advanced wear and breakdown of joint surfaces causing pain, grinding noises, and general joint dysfunction.
Hypermobility - Sometimes the joint becomes too loose and the posterior ligament is structured to allow the condyle and disc to advance forward beyond the socket. This can cause the jaw to lock open. This is sometimes called an "open lock".
Synovitis - The synovial lining, which produces lubrication to the joint, may become inflamed for a variety of reasons. This often causes an acutely tender and painful joint.
Treatment Options
Self help - This is usually the best option to begin with. Resting the jaw may be the best treatment so it can heal and regain stability. This may be accomplished by not clenching your teeth, practicing good posture, eating soft foods and reducing stress. Apply ice to the jaw for the first 24-48 hours after symptoms are noticed. Ice helps prevent swelling. Heat may be applied to tense and sore muscles. By application of heat, muscle spasms may be relieved. Exercise (passive) of the jaw regains normal range and function. It increases flexibility and strengthens muscles. This should be done as a passive exercise in contrast to eating hard foods which increases the stress on the joint. Medications such as Motrin, Advil, aspirin or other non-steroidal anti-inflammatory drugs reduce pain and inflammation.
Medications - Your doctor may prescribe muscle relaxants to decrease and control muscle spasms and muscle related pain. Non-steroidal anti-inflammatory drugs may be prescribed to reduce inflammation and control discomfort. Drugs to help control bruxism or grinding of the teeth may be recommended.
Physical therapy - You may be referred to a licensed physical therapist to help in the management of your disorder. Physical therapy promotes healing and reduces pain, swelling, and inflammation. It greatly improves jaw range of motion and muscle relaxation. Physical therapy techniques may include jaw exercises, posture training, mobilization of joints, ultrasound, and electrical stimulation to regain harmony to your jaw joints and muscles.
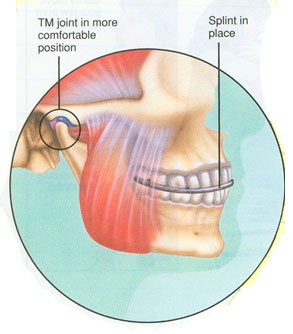 Splint therapy - It may be recommended that you wear a splint which is a clear plastic appliance. It fits over your teeth to help establish harmony between your muscles and joints. Splints primarily aid in stabilization of the bite and prevention and controlling bruxism and clenching. Most splints are constructed by your general dentist or a dentist who specializes in non-surgical TMJ management. Most splint therapy lasts for 1-3 months or more. A bruxism splint is worn primarily at night to aid in grinding and clenching habits. It helps reduce muscle tension and discomfort. An orthopedic stabilization splint lets your jaw move in the correct position, stabilizes the bite, relaxes musculature and reduces pressure on the TMJ. Proper wearing of your splint as directed by your doctor is most important in the treatment of your dysfunction. In the illustration at right the splint is in place between the upper lower teeth. It will act to perfect the bite artificially and prevent excessive force from being transmitted to the TMJ as the patient clenches or grinds. It will help with force dissipation even in the absence of these parafunctional activities and encourages the joints to repair themselves. The greatest advantages of this therapy are that most people will be helped to some degree, and the therapy is safe and reversible. Splint therapy - It may be recommended that you wear a splint which is a clear plastic appliance. It fits over your teeth to help establish harmony between your muscles and joints. Splints primarily aid in stabilization of the bite and prevention and controlling bruxism and clenching. Most splints are constructed by your general dentist or a dentist who specializes in non-surgical TMJ management. Most splint therapy lasts for 1-3 months or more. A bruxism splint is worn primarily at night to aid in grinding and clenching habits. It helps reduce muscle tension and discomfort. An orthopedic stabilization splint lets your jaw move in the correct position, stabilizes the bite, relaxes musculature and reduces pressure on the TMJ. Proper wearing of your splint as directed by your doctor is most important in the treatment of your dysfunction. In the illustration at right the splint is in place between the upper lower teeth. It will act to perfect the bite artificially and prevent excessive force from being transmitted to the TMJ as the patient clenches or grinds. It will help with force dissipation even in the absence of these parafunctional activities and encourages the joints to repair themselves. The greatest advantages of this therapy are that most people will be helped to some degree, and the therapy is safe and reversible.
Occlusal bite correction - If your TMJ disorder is caused or greatly effected by the way your teeth fit together, it may be necessary to correct your occlusion. You may need orthodontics (braces) to reposition your teeth in order to establish a stable bite. If your bite problem is primarily due to a malalignment of the jaws or a discrepancy between the upper and lower jaws you might need orthognathic surgery. This would realign the upper and lower jaws (usually in combination with orthodontics) to create a stable occlusion. Restorative dental procedures may be necessary by your general dentist to replace missing teeth, repair existing teeth or change the shape and size of teeth.
TMJ surgery - With other modalities of treatment available, surgery is reserved for those cases which fail to satisfactorily respond to the above mentioned methods. In some cases, the joint undergoes some degree of internal joint derangement and fails to respond to non-surgical treatment. Surgery is usually indicated if non-surgical treatments have failed and clinical and diagnostic findings indicate a derangement inside the TMJ. The following are several different types of TMJ surgery.
Lysis and lavage - This is a hydraulic distension and flushing of the joint with sterile saline and/or medications to increase the mobilization of the joint. If the disc has become adhered to the fossa surface or locked for a short period of time, this procedure may remobilize the disc. Lysis and lavage is an office procedure performed under IV sedation, which may be used to decrease discomfort and inflammation.
Arthroscopic arthroplasty surgery - This procedure is similar to arthroscopic surgery performed by orthopedic surgeons on the knee and other joints. This procedure is usually done in a hospital setting and requires a general anesthesia and is routinely done on an outpatient basis. Most TMJ derangements can be initially treated by arthroscopic surgery. Arthroscopic arthroplasty can be done as a diagnostic tool if diagnosis is uncertain and non-surgical treatments have failed. Adhesions and scarring may be removed to increase joint mobility. If the disc is displaced, causing painful popping or locking, a repositioning procedure can be accomplished arthroscopically. Until the last several years, this required an open joint procedure but with the current state of the arthroscopic "art", many discal repositioning procedures including suturing of the disc itself, are performed without open surgery. In cases of more severe degeneration such as torn discs, discs with holes worn in them, or arthritic and generative joints, arthroscopic surgery is highly effective. This procedure requires a small 3mm incision over the joint in front of the ear. Through this incision, the arthroscope is inserted into the joint space. Additional needles may be placed to perform the necessary procedures.
Open joint reconstructive surgery - If the joint fails to respond to the arthroscopic procedure or the condition is such that arthroscopy is not indicated, an open procedure is sometimes recommended. Under direct visualization the joint is reconstructed by smoothing the joint surfaces, repair of disc abnormality and removal of diseased tissue. A graft or artificial replacement of one or more joint surfaces may be used in the reconstruction of the joint. This procedure requires general anesthesia as well as an overnight stay in the hospital.
Condylotomy - Sometimes the jaw is sectioned from inside the mouth and just below the condyle. This is done in certain situations to restore a stable occlusion, to decrease the pressure on the joint or to change the condyle position. This procedure requires having the jaws wired together for 7-14 days. It requires general anesthesia and an overnight stay in the hospital.
Follow up care after surgery - Post-operative instructions will be given to you by your doctor regarding care of your incisions, suture removal, diet, physical therapy, and medications. Medication will be given for pain control, muscle relaxation, and prevention of infection. Additionally, postoperative physical therapy is an integral part of the rehabilitation after treatment. One of our doctors is always on-call for problems or questions and a post-operative appointment is usually scheduled 1-15 days after the procedure.
|






 Complex Masticatory Muscles - Surrounding the joint are groups of muscles that contract and relax in harmony so the jaws function properly. When the muscles are relaxed and flexible, and not under stress, they work in harmony with the other parts of the TMJ complex.
Complex Masticatory Muscles - Surrounding the joint are groups of muscles that contract and relax in harmony so the jaws function properly. When the muscles are relaxed and flexible, and not under stress, they work in harmony with the other parts of the TMJ complex.
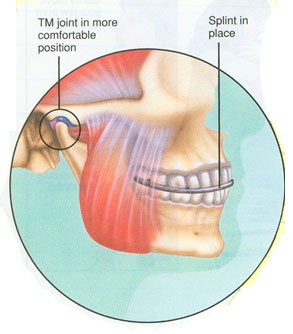 Splint therapy - It may be recommended that you wear a splint which is a clear plastic appliance. It fits over your teeth to help establish harmony between your muscles and joints. Splints primarily aid in stabilization of the bite and prevention and controlling bruxism and clenching. Most splints are constructed by your general dentist or a dentist who specializes in non-surgical TMJ management. Most splint therapy lasts for 1-3 months or more. A bruxism splint is worn primarily at night to aid in grinding and clenching habits. It helps reduce muscle tension and discomfort. An orthopedic stabilization splint lets your jaw move in the correct position, stabilizes the bite, relaxes musculature and reduces pressure on the TMJ. Proper wearing of your splint as directed by your doctor is most important in the treatment of your dysfunction. In the illustration at right the splint is in place between the upper lower teeth. It will act to perfect the bite artificially and prevent excessive force from being transmitted to the TMJ as the patient clenches or grinds. It will help with force dissipation even in the absence of these parafunctional activities and encourages the joints to repair themselves. The greatest advantages of this therapy are that most people will be helped to some degree, and the therapy is safe and reversible.
Splint therapy - It may be recommended that you wear a splint which is a clear plastic appliance. It fits over your teeth to help establish harmony between your muscles and joints. Splints primarily aid in stabilization of the bite and prevention and controlling bruxism and clenching. Most splints are constructed by your general dentist or a dentist who specializes in non-surgical TMJ management. Most splint therapy lasts for 1-3 months or more. A bruxism splint is worn primarily at night to aid in grinding and clenching habits. It helps reduce muscle tension and discomfort. An orthopedic stabilization splint lets your jaw move in the correct position, stabilizes the bite, relaxes musculature and reduces pressure on the TMJ. Proper wearing of your splint as directed by your doctor is most important in the treatment of your dysfunction. In the illustration at right the splint is in place between the upper lower teeth. It will act to perfect the bite artificially and prevent excessive force from being transmitted to the TMJ as the patient clenches or grinds. It will help with force dissipation even in the absence of these parafunctional activities and encourages the joints to repair themselves. The greatest advantages of this therapy are that most people will be helped to some degree, and the therapy is safe and reversible.